Living With Knee Osteoarthritis:
Effective Treatment and Management at Weaver Physio
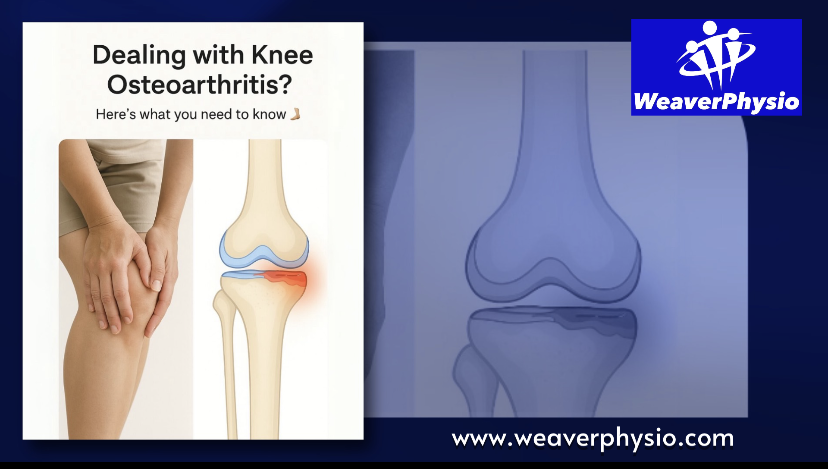
Struggling with knee pain that’s limiting your daily life? You’re not alone. Knee osteoarthritis (OA) is one of the most common causes of chronic joint pain in the UK, affecting millions of adults—especially those over 45. At Weaver Physio, we specialise in helping people across Cheshire live well with osteoarthritis, using proven physiotherapy and rehab strategies to reduce pain, improve movement, and regain control of their lives.
In this blog, we’ll break down exactly what knee osteoarthritis is, how it develops, what symptoms to watch for, and most importantly—how physiotherapy can help you manage it effectively and avoid surgery.
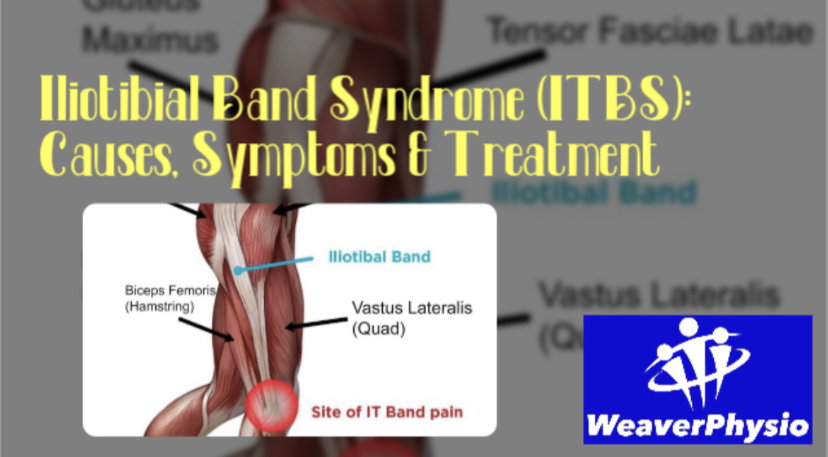
What Is Knee Osteoarthritis?
Knee osteoarthritis is a degenerative joint condition where the cartilage that cushions the bones in your knee slowly breaks down. As this protective cartilage wears away, bones begin to rub together, causing pain, swelling, stiffness, and reduced mobility.
Osteoarthritis is sometimes referred to as “wear and tear” arthritis, but it’s more complex than just ageing. In fact, many people in their 60s or older do not experience joint pain, while others may have severe symptoms in their 40s or 50s. The difference often lies in biomechanics, joint loading, previous injuries, activity levels, and weight.
What Causes Knee Osteoarthritis?
Several factors can increase your risk of developing knee OA:
• Age: Cartilage naturally wears with age, but not everyone develops symptoms.
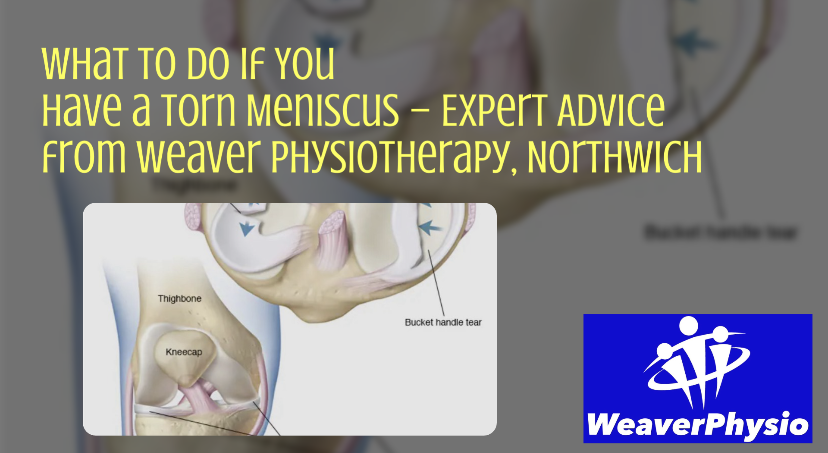
• Previous Injuries: Meniscal tears, ligament injuries (ACL), and fractures can predispose the knee to OA.
• Excess Weight: Every extra stone places around 4 times more pressure through the knee joint.
• Genetics: Family history may influence your joint structure and susceptibility.
• Occupational or Sporting Demands: Repetitive knee bending, kneeling, or heavy lifting can contribute.
• Biomechanical Issues: Poor alignment, muscle imbalances, or abnormal gait patterns can overload the joint.
Common Symptoms of Knee Osteoarthritis
Knee OA symptoms typically develop gradually and worsen over time. The most common complaints include:
• Persistent knee pain, especially during or after activity
• Morning stiffness, usually lasting less than 30 minutes
• Swelling or a feeling of fullness in the knee joint
• Clicking, grinding, or creaking (crepitus) during movement
• Reduced flexibility and range of motion
• Difficulty with activities like walking, climbing stairs, or standing up from sitting
• Joint instability or a feeling the knee may give way
If these symptoms sound familiar, early diagnosis and management can make a massive difference in your long-term outcomes.
Diagnosis and Clinical Assessment
At Weaver Physio in Northwich, our physiotherapists provide expert assessment and diagnosis of knee pain. We use a combination of:
• Detailed patient history
• Functional movement tests
• Joint mobility and strength assessment
• Gait analysis
• Referral for imaging (e.g., X-rays) if needed
Even if an X-ray shows “moderate to severe arthritis,” it doesn’t mean you’re doomed to joint replacement. We focus on function, not just structure, and many patients achieve significant pain relief and mobility improvements through physiotherapy alone.
How Physiotherapy Can Help Knee Osteoarthritis
While knee OA is not reversible, symptoms can be dramatically reduced through the right rehab approach. At Weaver Physio, we create personalised management plans that help you live an active, pain-free life—often avoiding surgery entirely.
Here’s how physiotherapy can make a real difference:
1. Strengthening Exercises
Strong muscles protect joints. In particular, the quadriceps, hamstrings, calves, and glutes play a critical role in supporting your knees.
We use targeted strengthening to:
• Reduce joint load and compressive forces
• Improve movement control and stability
• Relieve pain by improving the way your body moves
Progressive loading (starting light and gradually increasing resistance) helps build strength without flaring symptoms.
2. Manual Therapy and Joint Mobilisation
Our hands-on treatments can help:
• Ease joint stiffness
• Improve circulation
• Reduce pain and swelling
• Promote normal joint mechanics
Manual techniques are often combined with exercises to optimise outcomes.
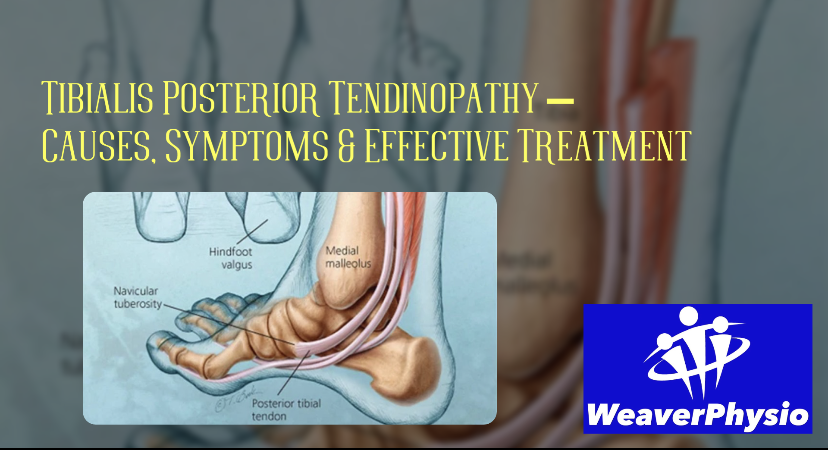
3. Gait Re-Education and Movement Analysis
Your walking pattern can put unnecessary strain on your knees. We assess and correct any abnormal mechanics to:
• Reduce limping
• Improve alignment and balance
• Minimise stress on the joint
We may also recommend orthotics or supportive footwear where appropriate.
4. Pain Relief Techniques
Our team uses a range of techniques to calm pain and inflammation:
• Taping or bracing to unload the joint
• Electrotherapy or acupuncture (when indicated)
• Cryotherapy or heat therapy depending on the stage of your symptoms
We always explain what works and why—no fads, no guesswork.
5. Education and Lifestyle Advice
We’ll help you understand:
• How to pace your activities to avoid flare-ups
• The role of weight loss in knee health
• How to modify your movements to protect the joint
• Why rest isn’t always the answer—and how gentle movement promotes healing
When you know what helps and what doesn’t, you’re back in control.
Other Helpful Treatments and Options
At Weaver Physio, we also offer additional supportive treatments:
🌀 Shockwave Therapy
Proven for soft tissue pain (e.g., pes anserine bursitis, patellar tendinopathy). It can help reduce pain around the knee when traditional treatment hasn’t worked.
🧊 Acupuncture
An effective way to reduce persistent pain and muscle tension.
🦵 IASTM (Instrument Assisted Soft Tissue Mobilisation)
Rockblades and similar tools help release tight fascia and promote tissue healing.
Common Myths About Knee Osteoarthritis
Let’s bust a few myths we hear regularly in clinic:
❌ “You should stop exercising.”
Wrong. Regular low-impact activity is one of the best ways to manage OA. Movement helps lubricate joints, strengthen muscles, and reduce pain.
❌ “If your X-ray shows arthritis, you’ll need a knee replacement.”
Not necessarily. Many people with severe imaging findings live active lives without surgery. It’s about function, not just pictures.
❌ “It’s just your age.”
While age is a factor, OA is not inevitable. Lifestyle, strength, and biomechanics play a huge role.
Safe & Effective Exercises for Knee OA
Here are a few examples we often recommend (under guidance):
1. Seated Knee Extensions – Strengthens quads without load
2. Bridges – Builds glute strength
3. Step-Ups – Functional strength
4. Wall Sits – Isometric strength with control
5. Mini Squats – Gradual return to full movement
6. Stationary Cycling – Excellent for mobility and fitness with low joint impact
We always tailor programs to your pain levels and physical capacity—there’s no one-size-fits-all approach.
When Is It Time to Consider Surgery?
Knee replacement may be considered when:
• Pain severely limits everyday function
• You’ve exhausted conservative treatment
• Quality of life is consistently poor
Even then, prehabilitation with physiotherapy helps improve surgical outcomes. And post-op rehab is critical to successful recovery.
At Weaver Physio, we support you before and after surgery to ensure the best possible results.
Real Results at Weaver Physio
We’ve helped hundreds of clients across Cheshire reduce their knee pain, improve their mobility, and delay or avoid surgery. From active retirees to manual workers, runners to gardeners—our approach works because it’s individualised, evidence-based, and always focused on what matters to you.
Don’t Let Knee Osteoarthritis Control Your Life
Knee OA can be frustrating and painful—but it doesn’t have to define your life. At Weaver Physio, we help you take charge of your symptoms with proven strategies that work in the real world. From personalised rehab to hands-on treatment, our experienced team is here to get you moving better, feeling stronger, and living pain-free.
Ready to take the first step?
Book an Appointment at Weaver Physio Today
Located in the heart of Northwich, Weaver Physiotherapy & Sports Injury Clinic is your trusted partner for expert osteoarthritis care in Cheshire.
👉 Visit http://www.weaverphysio.com
📞 Call us to book: 01606 227484
📧 Or email: weaverphysio@outlook.com
#KneeOsteoarthritis #KneePainRelief #CheshirePhysio #WeaverPhysio #JointHealth #OsteoarthritisTreatment #NorthwichPhysio #ActiveAging #PhysiotherapyWorks #LivePainFree #MobilityMatters #ArthritisAwareness #MoveBetter #StrongerKnees #JointCare #ShockwaveTherapy #AcupunctureForPain #OARehab #PersonalisedPhysio #ManualTherapy #StayActive