Iliotibial Band Syndrome (ITBS)
Causes, Symptoms & Treatment | Weaver Physiotherapy Northwich
Understanding Iliotibial Band Syndrome
If you’re a runner, cyclist, or active individual experiencing pain on the outer side of your knee or thigh, you could be dealing with Iliotibial Band Syndrome (ITBS) — one of the most common causes of lateral knee pain in athletes.
At Weaver Physiotherapy & Sports Injury Clinic in Northwich, Cheshire, our team of Chartered Physiotherapists specialises in diagnosing and treating Iliotibial Band Syndrome, helping runners and athletes of all levels recover quickly, move freely, and prevent recurrence.
With over 70 years of combined clinical experience, our physiotherapists combine hands-on treatment, advanced rehabilitation, and movement re-education to tackle ITBS at its source.
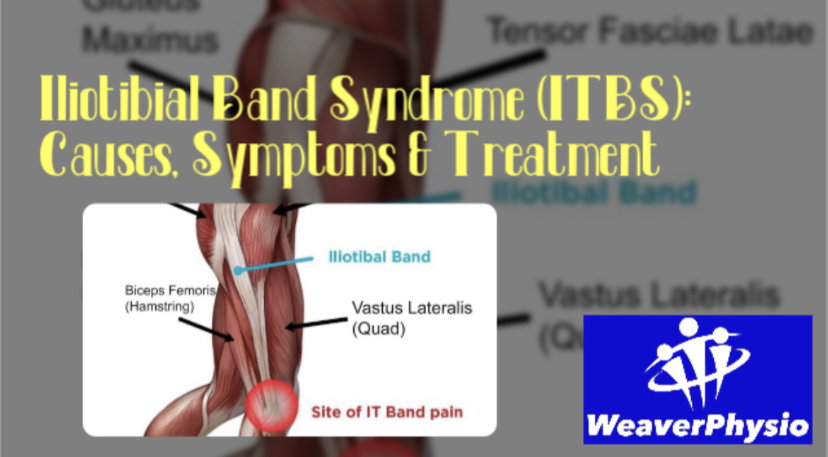
What Is the Iliotibial Band?
The iliotibial band (ITB) is a thick band of connective tissue that runs from the hip to the outer side of the knee, connecting the tensor fasciae latae (TFL) and gluteus maximus muscles to the tibia (shin bone). Its role is to stabilise the knee and hip during movement, particularly when running, walking, or cycling.
When functioning properly, the IT band glides smoothly over the bony structures around the knee. However, if it becomes tight, inflamed, or irritated from repetitive friction, it can cause pain on the outside of the knee — the hallmark of Iliotibial Band Syndrome.
What Causes Iliotibial Band Syndrome?
ITBS is an overuse injury, meaning it develops gradually from repetitive stress rather than a single traumatic event. The condition is especially common among runners, cyclists, hikers, and gym-goers who perform frequent bending and straightening of the knee.
Common Causes Include:
1. Overtraining or Sudden Increase in Activity
Increasing your mileage, pace, or hill training too quickly can overload the IT band and surrounding structures.
2. Muscle Imbalances and Weakness
Weak gluteal or hip stabilising muscles cause the IT band to take on excessive tension, leading to irritation around the knee.
3. Tightness in the IT Band or Hip Muscles
Limited flexibility in the TFL, glutes, or quadriceps can increase friction along the IT band.
4. Poor Running Form or Biomechanics
Excessive inward knee movement (valgus), overstriding, or poor hip control can increase stress on the outer knee.
5. Improper Footwear or Running Surface
Worn-out shoes, excessive camber (running on sloped surfaces), or running always in one direction can contribute to ITBS.
6. Leg Length Discrepancy or Pelvic Alignment Issues
Subtle biomechanical differences can lead to uneven stress distribution across the knees and hips.
Who Is Most at Risk?
Iliotibial Band Syndrome can affect anyone who is active, but some groups are particularly prone to it:
• Distance runners, especially those training for marathons or half-marathons
• Cyclists with poor bike setup or excessive mileage
• Hikers tackling long or uneven terrain
• Footballers, rugby players, and gym-goers doing repetitive squatting or lunging
• Office workers with tight hip flexors or glutes due to prolonged sitting
If you’re training hard but developing sharp or aching pain on the outside of your knee, you may be in the early stages of ITBS.
Symptoms of Iliotibial Band Syndrome
The hallmark symptom of ITBS is pain on the outer (lateral) side of the knee, but the condition can cause a range of sensations and discomfort patterns.
Common Symptoms Include:
• Sharp or burning pain on the outside of the knee
• Pain that worsens with running, especially downhill or after several miles
• Discomfort when climbing stairs or getting up from a seated position
• Tightness or tenderness along the outer thigh
• Snapping or clicking sensation around the knee
• Pain that may radiate up towards the hip or down the leg
The pain often starts gradually and worsens with continued activity. Early intervention is crucial to prevent the condition from becoming chronic.
How Is Iliotibial Band Syndrome Diagnosed?
At Weaver Physiotherapy, our expert clinicians take a comprehensive approach to diagnosis. We don’t just treat the pain — we identify the underlying cause.
Our ITBS Assessment Includes:
1. Detailed Case History
Understanding your training habits, footwear, injury history, and lifestyle factors.
2. Physical Examination
Assessing hip, knee, and ankle alignment, as well as muscle strength and flexibility.
3. Movement Analysis
Evaluating running gait, walking pattern, or cycling posture to identify mechanical contributors.
4. Palpation & Orthopaedic Tests
Testing specific structures to rule out other causes of knee pain (e.g., meniscus injury, lateral ligament strain).
5. Video Gait Analysis
Using slow-motion technology to spot subtle biomechanical issues that lead to ITB irritation.
This holistic assessment ensures your treatment plan is tailored to your individual needs and the root cause of your problem.
Physiotherapy Treatment for Iliotibial Band Syndrome
1. Pain Relief and Inflammation Management
The first goal is to reduce pain and inflammation. Your physiotherapist may use:
• Manual therapy and soft tissue release to ease tension along the IT band and surrounding muscles.
• Ice therapy or ultrasound for inflammation control.
• Kinesiology taping to offload the IT band and support healing.
2. Deep Tissue and Sports Massage
Massage therapy is extremely effective in reducing IT band tightness. At Weaver Physio, our Sports Massage and Deep Tissue Massage treatments target the TFL, glutes, quadriceps, and lateral thigh to restore normal tissue mobility and reduce friction at the knee.
3. Shockwave Therapy
For chronic or stubborn cases, Shockwave Therapy provides a powerful, evidence-based solution. It uses acoustic waves to stimulate blood flow, break down scar tissue, and accelerate healing in the IT band and surrounding tendons. NICE (National Institute for Health and Care Excellence) recommends this treatment for persistent soft tissue conditions.
4. Strength & Conditioning Rehabilitation
Once pain is under control, strengthening exercises are essential to correct underlying imbalances. Your physiotherapist will design a tailored exercise program targeting:
• Gluteus medius and maximus (hip stabilisers)
• Core muscles (for pelvic control)
• Hamstrings and quadriceps (to balance knee mechanics)
5. Gait Re-Education
Poor running form often drives ITBS. Our Runner’s MOT and Video Gait Analysis sessions identify biomechanical inefficiencies, helping you adjust stride length, cadence, and posture for long-term prevention.
6. Stretching and Mobility Work
Specific stretches for the IT band, TFL, glutes, and quads help relieve tension and maintain flexibility. Foam rolling and mobility drills may also be prescribed.
7. Return to Sport Planning
We guide you safely back into training with progressive loading, ensuring your tissue capacity matches your running or cycling demands.
At Weaver Physio, your treatment plan is completely individualised — addressing pain relief, restoring function, and preventing recurrence.
Exercises for Iliotibial Band Syndrome
Here are a few examples of physiotherapy-approved exercises often included in recovery plans:
1. Side-Lying Leg Raises – Strengthens the gluteus medius.
2. Clamshells – Targets hip stabilisers and improves knee alignment.
3. Hip Bridges – Builds glute strength and reduces ITB tension.
4. Foam Rolling the IT Band – Helps release tight fascia and improve mobility.
5. Standing IT Band Stretch – Gently lengthens the lateral thigh structures.
(Always consult your physiotherapist before starting new exercises, as incorrect technique can worsen symptoms.)
How Long Does Recovery Take?
Recovery time depends on severity, chronicity, and training load, but most patients improve significantly within 4–8 weeks of structured physiotherapy and activity modification. Chronic or long-standing cases may take longer, especially if biomechanical retraining is needed.
Our goal at Weaver Physio is to not only get you pain-free, but also to build resilience so you can return to running, cycling, or sport with confidence — and without fear of re-injury.
Preventing Iliotibial Band Syndrome
1. Gradual Training Progression
Avoid sudden increases in distance, pace, or hill work. Follow the 10% rule – increase weekly mileage by no more than 10%.
2. Strengthen Your Glutes & Core
Regular hip and core strengthening reduces ITB strain during movement.
3. Prioritise Flexibility
Incorporate regular stretching and foam rolling of the IT band, quadriceps, hamstrings, and calves.
4. Check Your Footwear
Replace worn-out shoes and ensure your trainers match your running style. Gait analysis can identify whether you need neutral or stability shoes.
5. Cross-Train & Rest
Include low-impact activities like swimming or cycling, and schedule adequate rest days to allow tissue recovery.
6. Get a Professional Running Assessment
Our Runner’s MOT identifies inefficiencies in your stride and recommends personalised corrective exercises — ideal for injury prevention and performance enhancement.
Why Choose Weaver Physiotherapy for IT Band Syndrome Treatment?
At Weaver Physiotherapy & Sports Injury Clinic, we’re passionate about helping runners, athletes, and active individuals overcome injury and return to what they love.
What Sets Us Apart:
✅ Specialist Running Injury Clinic – Experts in ITBS, runner’s knee, Achilles pain, and shin splints
✅ 70+ Years Combined Experience – Trusted Chartered Physiotherapists in Cheshire
✅ Comprehensive Assessment – Including video gait analysis and functional testing
✅ Advanced Treatments – Shockwave therapy, acupuncture, sports massage, rehab & manual therapy
✅ Tailored Rehabilitation Plans – Designed around your sport, goals, and lifestyle
✅ Local, Trusted Experts – Serving Northwich, Knutsford, Winsford, Middlewich, Frodsham & Tarporley
Whether you’re a Parkrunner, marathoner, or simply love staying active, our mission is to help you move better, perform better, and live pain-free.
Take Control of Your Recovery Today
Don’t let IT band pain stop you from doing what you love. Early intervention is key — the sooner you seek help, the faster you’ll recover.
📞 Call Weaver Physiotherapy & Sports Injury Clinic today on 01606 227484
🌐 Book online at https://www.weaverphysio.com
📍 Weaver Physio – Your Trusted Partner in Recovery, Performance & Pain-Free Living