Tibialis Posterior Tendinopathy
Causes, Symptoms & Effective Treatment | Weaver Physiotherapy, Northwich
If you’ve been struggling with persistent pain or swelling around the inside of your ankle, especially when walking or running, you may be suffering from Tibialis Posterior Tendinopathy (TPT) — a common but often underdiagnosed cause of foot and ankle pain.
At Weaver Physiotherapy & Sports Injury Clinic in Northwich, Cheshire, our expert physiotherapists specialise in diagnosing and treating this condition using evidence-based rehabilitation, manual therapy, orthotics, and strengthening techniques — helping you return to pain-free movement and prevent further complications such as flat foot deformity.
🦶 What is Tibialis Posterior Tendinopathy?
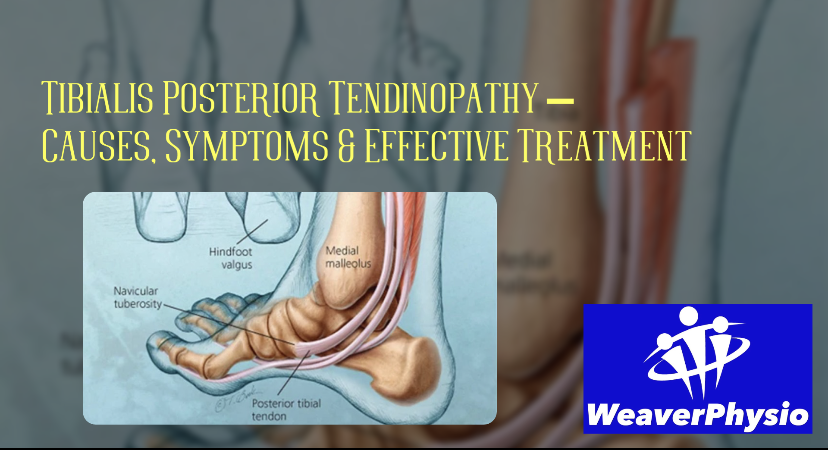
The tibialis posterior is a key muscle located deep in your lower leg, running behind the inner ankle bone (medial malleolus) and attaching to the underside of the foot. Its primary roles are to:
• Support the arch of the foot
• Assist with inversion (turning the foot inward)
• Aid in plantarflexion (pointing the toes down) during walking and running
Tibialis Posterior Tendinopathy occurs when the tendon becomes overloaded, irritated, or degenerated, leading to inflammation, pain, and loss of function. It’s one of the leading causes of adult-acquired flatfoot deformity, especially in active individuals and middle-aged adults.
⚠️ Common Causes and Risk Factors
Like most tendon injuries, tibialis posterior tendinopathy usually results from repetitive strain or biomechanical overload rather than a single traumatic event. Common contributing factors include:
1. Overuse and Training Errors
• Sudden increases in training volume or intensity (e.g., long runs, hill work, plyometrics)
• Excessive walking or standing, particularly on hard surfaces
• Poor recovery between sessions
2. Biomechanical Factors
• Over-pronation (collapsed arches or “flat feet”)
• Weakness in the foot intrinsic muscles or calf
• Reduced ankle mobility or stiffness
3. Footwear Problems
• Worn-out shoes with poor arch support
• Unsuitable footwear for activity or running style
4. Systemic and Age-Related Changes
• Tendon degeneration with age (tendinosis)
• Inflammatory conditions such as rheumatoid arthritis
• Obesity, diabetes, or high cholesterol
At Weaver Physio, our clinicians often see tibialis posterior issues linked to poor foot mechanics and running gait, which can be accurately assessed through our Video Gait Analysis and Runner’s MOT service.
🔍 Symptoms of Tibialis Posterior Tendinopathy
The symptoms typically develop gradually and may worsen with activity. You might experience:
• Pain or tenderness along the inside of the ankle and foot, especially behind the bony bump (medial malleolus)
• Swelling along the tendon
• Pain when standing on tiptoes or turning the foot inwards
• A noticeable flattening of the arch or rolling in of the ankle
• Difficulty walking or running, especially on uneven ground
• In more advanced cases, visible foot deformity or “fallen arch” appearance
Early diagnosis and treatment are crucial — once the tendon becomes elongated or the arch collapses, recovery can take significantly longer.
🧠 How is Tibialis Posterior Tendinopathy Diagnosed?
At Weaver Physiotherapy & Sports Injury Clinic, diagnosis begins with a detailed clinical assessment:
1. Patient History – discussing pain location, onset, footwear, training habits, and medical background
2. Physical Examination – palpation along the tendon, checking arch height, strength testing, and observing gait
3. Functional Tests – single-leg heel raise, foot posture index, and load tolerance
4. Imaging (if required) – Ultrasound or MRI can confirm tendon thickening, tears, or degeneration
Our specialist physiotherapists use this information to identify the root cause and tailor a treatment plan specific to your condition and lifestyle.
💪 Physiotherapy Treatment for Tibialis Posterior Tendinopathy
Physiotherapy is the gold standard treatment for tibialis posterior tendinopathy. At Weaver Physio, we use a combination of hands-on therapy, exercise prescription, and advanced techniques to ensure full recovery and long-term prevention.
1. Load Management & Activity Modification
Initially, it’s important to reduce tendon stress to allow healing.
• Avoid aggravating activities (running, jumping, long walks on uneven surfaces).
• Replace high-impact exercise with low-impact options such as cycling or swimming.
• Use supportive footwear or orthotics to reduce load on the tendon.
Our physiotherapists will help you find the right balance between rest and controlled loading — essential for tendon recovery.
2. Pain Management & Early Rehabilitation
• Manual therapy & massage to reduce tension in the calf and surrounding tissues
• Taping or bracing to support the arch and unload the tendon
• Shockwave Therapy for chronic tendinopathy to stimulate healing and collagen regeneration
• Acupuncture may also help reduce pain and inflammation
These treatments help create the right environment for tissue repair before progressing to strengthening.
3. Progressive Strengthening Exercises
A key element in recovery is gradual tendon loading through targeted exercise.
Typical exercises include:
• Isometric heel raises (holding the position for tendon load without movement)
• Eccentric heel drops to build tendon resilience
• Resistance band inversion to strengthen tibialis posterior
• Single-leg balance and stability work
Our team will tailor your rehabilitation plan to your stage of recovery, ensuring safe progression.
4. Gait Retraining & Biomechanical Correction
Through Video Gait Analysis, our physiotherapists can identify issues such as over-pronation, hip weakness, or stride inefficiency that may be contributing to your condition.
Corrections may involve:
• Adjusting running technique
• Strengthening glutes and core
• Modifying cadence or foot strike pattern
This approach prevents recurrence and improves overall movement efficiency.
5. Orthotics & Footwear Advice
Custom or semi-custom orthotics can help restore proper foot alignment and offload the tibialis posterior tendon.
We often recommend:
• Supportive trainers with firm heel counters
• Arch-support inserts or motion-control shoes
• Avoiding minimalist or overly flexible footwear during rehabilitation
6. Shockwave Therapy at Weaver Physio
For chronic or stubborn tibialis posterior tendinopathy, Radial Shockwave Therapy (RSWT) is an excellent option.
Shockwave delivers high-energy sound waves into the affected tendon to:
• Stimulate blood flow
• Break down scar tissue
• Promote tendon healing
• Accelerate pain relief
This treatment is clinically proven and recommended by NICE (National Institute for Health and Care Excellence). Many patients notice significant improvement after just 3–5 sessions at Weaver Physio.
⏳ Expected Recovery Time
Recovery time depends on the severity and duration of the condition.
• Mild tendinopathy: 6–8 weeks with structured rehab
• Moderate tendon degeneration: 8–16 weeks
• Chronic or severe cases with flatfoot changes: 4–6 months
Consistency with your rehabilitation exercises and footwear support is key to long-term success.
🧩 Long-Term Management and Prevention
Once symptoms improve, your focus should shift to maintaining tendon health and preventing recurrence.
Our physiotherapists will guide you through:
• Ongoing strength and conditioning of the foot and calf muscles
• Flexibility routines for calves and Achilles
• Regular review of footwear and orthotics
• Gradual return to running or sport with progressive loading
For runners, we also recommend periodic Runner’s MOT or Gait Analysis sessions to catch early biomechanical changes before pain returns.
🏃♂️ Can Runners Get Tibialis Posterior Tendinopathy?
Absolutely — this is a common overuse injury in runners, especially those:
• Training on hard or cambered surfaces
• Increasing mileage too quickly
• Wearing unsupportive or worn shoes
• With weak calf or hip stabilisers
At Weaver Physio, we treat many runners suffering from inner ankle pain that turns out to be tibialis posterior tendinopathy. Addressing strength, mobility, and running form is essential to get you back running stronger and pain-free.
🧬 The Difference Between Tendinitis and Tendinopathy
You might see the terms “tendinitis” and “tendinopathy” used interchangeably — but they describe different stages of the same problem:
• Tendinitis – early, acute inflammation phase
• Tendinopathy – later degenerative phase with collagen breakdown and reduced healing
Understanding this difference helps us choose the right treatment — moving away from just rest and anti-inflammatories towards progressive strengthening and tissue remodelling.
🏥 Why Choose Weaver Physiotherapy for Tendon Pain?
With over 70 years of combined clinical experience, our Chartered Physiotherapists are specialists in diagnosing and treating complex foot and ankle conditions.
At Weaver Physiotherapy & Sports Injury Clinic in Northwich, Cheshire, we provide:
• Expert physiotherapy for tendon injuries
• Shockwave Therapy for stubborn or chronic cases
• Video Gait Analysis & Runner’s MOT to identify root causes
• Tailored rehabilitation & strength programmes
• Sports massage & manual therapy for pain relief and flexibility
We help patients across Northwich, Knutsford, Winsford, Middlewich, Frodsham, Tarporley, and Cheshire recover from tendon injuries and stay active for life.
📞 Book Your Appointment Today
Don’t let foot or ankle pain hold you back. Early treatment can prevent long-term tendon damage and arch collapse.
📍 Visit Weaver Physiotherapy & Sports Injury Clinic, Northwich
📞 Call 01606 227484
🌐 Book online at https://www.weaverphysio.com
Let our team help you recover, strengthen, and get back to doing what you love — pain-free.